Dementia¶
Thomas Horton
Background¶
- Alzheimer’s Disease (AD): short-term memory deficits prominent
- Vascular Dementia: “Stepwise decline” in memory and functional status
- Lewy Body Dementia: hallucinations, memory difficulties with atypical Parkinsonism early
- Frontotemporal Dementia: behavioral (aggressive or disinhibited), language (primary progressive aphasias) or memory (Alzheimer’s/FTD overlap) variants
- Posterior Cortical Atrophy: visual difficulties and ocular apraxia preceding memory problems
- Creutzfeldt-Jakob Disease (CJD): manifests with subacute cognitive decline, seizures, vision loss, personality changes. Can develop startle myoclonus
- Corticobasal degeneration: focal neurologic changes with parkinsonism
- Neurosyphilis: rare, but treatable, present with a range of cognitive changes. Develop meningovascular encephalitis. Pts can develop an arteritis, headache, and hydrocephalus.
- Normal Pressure Hydrocephalus (NPH): “wet, wacky and wobbly” meaning incontinence, gait apraxia and cognitive changes (usually frontal symptoms)
- Autoimmune Dementias: includes limbic encephalitis (like NMDA) where there are memory and personality changes, autonomic changes, hallucinations, and seizures
| Normal Aging | Mild Cognitive Impairment | Alzheimer’s Dementia (DSM V Diagnostic Crit.) |
|---|---|---|
Mild decline in working memory More effort/time needed to recall new info New learning slowed but well compensated by lists, calendars, etc. + No impairment in social & occupation functioning |
Subjective complaint of cognitive decline in at least one domain + Cognitive decline is noticeable and measurable + No impairment in social & occupation functioning |
Evidence of significant cognitive decline from a previous level of performance in one or more cognitive domains + Causes significant impairment in social & occupation functioning + Other medical & psychiatric conditions, including delirium, have been excluded + Insidious onset and gradual progression of impairment in at least two cognitive domains |
| Cognitive domains: learning/memory, language, executive function, complex attention, perceptual motor, social cognition | ||
| Alzheimer’s Disease | Vascular Dementia | Lewy Body Dementia | Frontotemporal Dementia | |
|---|---|---|---|---|
| Onset | Gradual | Sudden or stepwise | Gradual | Gradual (age < 60) |
| Cognitive Domains & Symptoms | Memory, language, visuospatial | Depends on location of ischemia | Memory, visuospatial | Executive dysfunction, personality changes, disinhibition, language, +/- memory |
| Motor Symptoms | Rare early Apraxia later |
Correlates with ischemia | Parkinsonism | None |
| Progression | Gradual (over 8-10 years) | Gradual or stepwise with further ischemia | Gradual, but faster than Alzheimer’s disease | Gradual, but faster than Alzheimer’s disease |
| Imaging | Possible global atrophy | Cortical or subcortical on MRI | Possible global atrophy | Atrophy in frontal & temporal lobes |
Evaluation¶
- MINI-COG: Screening test for cognitive impairment (highly sensitive)
- Ask pt to remember three words (banana, sunrise, chair). Ask pt to repeat immediately
- Ask pt to draw clock. After numbers are on the face, ask pt to “set
hands to 10 past 11”
- Correct is all numbers in right position AND hands pointing to the 11 and the 2
- Ask pt to recall the three words
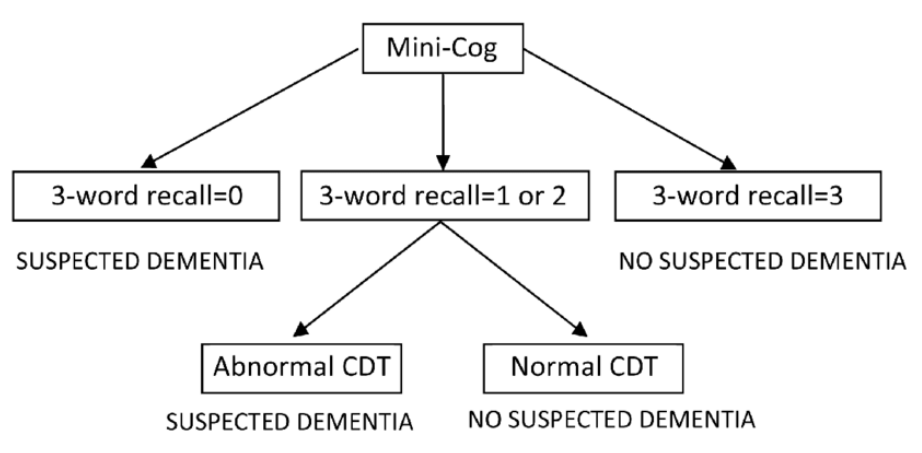
MINI-COG Flowchart
-
MOCA: Montreal Cognitive Assessment
- Lengthier test of cognition (but highly specific for cognitive impairment)
- Useful for detecting subtle deficits as in Mild Cognitive Impairment (MCI)
- Scores:
- 18-25: Mild cognitive impairment
- 10-17: Moderate cognitive impairment
- <10: Severe cognitive impairment
-
Rule out reversible causes of dementia-like symptoms: DEMENTIA
- Drugs
- Emotional (depression)
- Metabolic (CHF, COPD, CKD, OSA)
- Endocrine (hypothyroidism, hyperparathyroidism, hyponatremia)
- Nutrition (B12 deficiency)
- Trauma (chronic SDH)
- Infection
- Arterial (vascular)
- B12, thyroid studies
- RPR, HIV testing in at-risk patient groups
- Neuropsych testing can be done for more clear patterns of dysfunction
- MRI brain with contrast if concerned for inflammatory or infectious
causes
- CJD: cortical ribboning on DWI with T2 hyperintensity in the thalamus and basal ganglia
- Sulcal crowding and bowing of the corpus callosum can be seen in NPH on imaging
Management¶
- Targeting Cognitive Impairment
- Cholinesterase Inhibitors: Donepezil, rivastigmine
- Indicated for any stage (except FTD)
- SE: GI (nausea, diarrhea), bradycardia, orthostasis
- NMDA antagonists: Memantine
- Indicated in moderate to severe AD in combination with cholinesterase inhibitors
- Fewer SE than cholinergic medications
- Cholinesterase Inhibitors: Donepezil, rivastigmine
- Vitamin supplementation (i.e. Vitamin E)
- Unclear benefit in delaying progression of dementia
- Targeting Behaviors
- Non-pharmacologic management has the best evidence of effectiveness
- Depression: Treat with antidepressants (SSRI’s)
- Sleep Disturbance: Mirtazapine (7.5 mg nightly) or Trazodone (25 mg nightly)
- Agitation: Try SSRI (citalopram, sertraline)
- Consider antipsychotics (black box warning increased risk of death in elderly)