Asthma¶
Jared Freitas
Background¶
- Typically diagnosed in childhood, but occupational asthma, aspirin-induced asthma and eosinophilic asthma are more commonly diagnosed in adults
- Three most common symptoms: wheezing after trigger, nighttime cough, and associated dyspnea
- COPD-asthma overlap syndromes: newer entity that typically involves
intermittent symptoms
- Obstruction is present but does not fully resolve with bronchodilator
- Consider this diagnosis in a pt w/significant smoking history who is dx’d with asthma at age >40yo
Evaluation¶
- Ask about triggers: cold, exercise, URIs, allergens, inhaled irritants
- Ask about family history or personal history of atopy, eczema, allergic rhinitis
- Exam: wheezing, prolonged expiratory phase; nasal polyps, rhinitis, eczema
- Spirometry (PFT’s) with reversible obstruction
- FEV1/FVC <0.7; FEV1 12% and 200 mL after bronchodilator
- “All That Wheezes Is Not Asthma”. Must rule out alternative
diagnoses:
- Panic attacks, upper airway obstruction, foreign body, vocal cord dysfunction, CHF (cardiac asthma), COPD, ILD
- Consider CBC w/diff to screen for significant anemia and eosinophilia (associated w/allergic asthma or eosinophilic pneumonia)
- If concerned for allergic asthma or allergic bronchopulmonary aspergillosis, consider measuring total serum IgE levels
Classify Severity and Assess for Symptom Control with the RULE OF 2s¶
- Does the patient have symptoms or require rescue inhaler ≥2 times per week?
- Does the patient endorse nighttime symptoms ≥ 2 times per month?
- Does the patient have to refill rescue inhaler ≥ 2 times per year?
- Does the patient ever have to limit activity due to asthma symptoms?
Initial Assessment of Severity¶
- Intermittent: No to all of the above and FEV1> 80% predicted. Start at step 1
- Persistent: Yes to any question above. Start at Step 2
- Mild: Less than daily symptoms, less than weekly nighttime symptoms, minor limitation to activities. FEV >80% predicted
- Moderate: Daily symptoms, weekly nighttime symptoms, some limitation to activities. FEV 60-80% predicted
- Severe: More severe symptoms than above, FEV1 <60% predicted
- Consider referral to pulmonary
Management¶
- Aim to use the lowest possible step to maintain symptom control. Also consider stepping down therapy if pt has been well-controlled for >3 months
- Prior to escalating therapy, consider:
- Adherence to therapy (including inhaler technique), uncontrolled comorbidities (allergies, GERD, OSA, etc), and alternative diagnoses
- Ensure patients receive MDI and spacer teaching for full effect
- Updated Guidelines: prn ICS - LABA > prn SABA Step 1 (mild
intermittent) and Step 2 (mild persistent)
- Reduces exacerbations, easier to schedule does in future if needed
- SYGMA Trial showed rescue/prn Budesonide-formoterol (ICS - LABA) non-inferior to daily ICS-LABA + prn SABA in preventing exacerbations
- Follow-up
- Repeat PFTs q3-6 mos after beginning therapy and q1-2 yrs thereafter
- Regular follow up at least q6 mos for all patients with asthma
VA specific guidance¶
- Mometasone is the formulary ICS and Wixela (fluticasone-salmeterol) is the formulary ICS/LABA
- Ordering PFTs: Refer to Pulm section on PFTs for VUMC and VA specifics
- Please see above text for updated guidance on using prn ICS – LABA for step 1/step 2
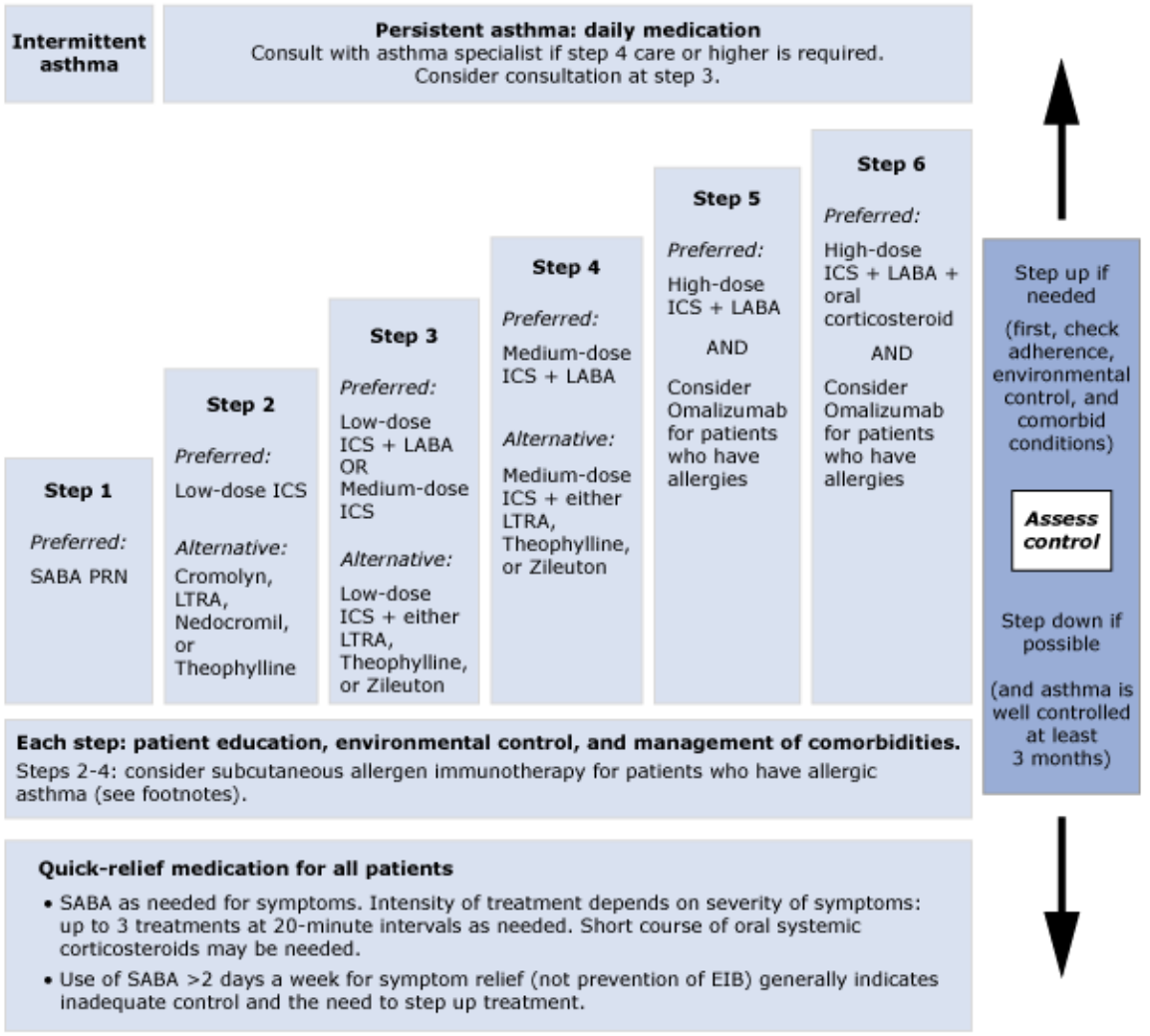
Image by National Heart, Blood, and Lung Institute. Distributed under a CC BY 2.5 license.
Last update:
2022-07-05 14:41:01