Lipids¶
Brittany Saldivar
Background¶
-
1º Prevention: pts at increased risk who have not yet had a vascular event
-
2º Prevention: pts with pre-existing occlusive vascular disease or ASCVD (e.g., stroke, TIA, CAD + angina, ACS, coronary or arterial revascularization, PAD)
-
Screening: USPSTF 2016 Guidelines: q5years for adults 40-75yrs
-
ACC/AHA 2019 Guideline: adults 20-39 q 4-6yrs; <21yrs if strong fam hx; 40-75 “routinely” assess CV risk and calculate 10 yr ASCVD risk (lipid pnl q3-12 months)
-
Dot phrase: .ASCVD2013
-
Evaluation¶
-
Fasting vs Non-Fasting Lipid Panel
- Triglycerides are most impacted by non-fasting testing which can artificially lower LDL-C depending on how the laboratory measures/calculates LDL. Consider fasting lipid panels when triglyceride levels are high
-
Consider 2º causes of HLD in initial workup: hypothyroidism, DM, EtOH use, smoking, liver disease, nephrotic syndrome, CKD, meds (e.g., thiazide, glucocorticoids)
Management¶
-
Lifestyle changes:
-
Heart Healthy Diet: ↓ trans/saturated fats, choose skim milk, low-fat dairy products
-
Emphasizes fruits, vegetables, whole grains, poultry, fish, nuts and olive oil, while limiting red and processed meats, sodium and sugar-sweetened foods and beverages
-
Promote a healthy weight, regular exercise, smoking cessation, limit EtOH
Statin Therapy
-
Initiate as outlined in the following algorithms
-
Check AST/ALT prior to initiation
-
Note that PCE used to estimate ASCVD risk is best validated for non-Hispanic whites and blacks. Consider use of additional risk prediction tools/factors in other patient populations
-
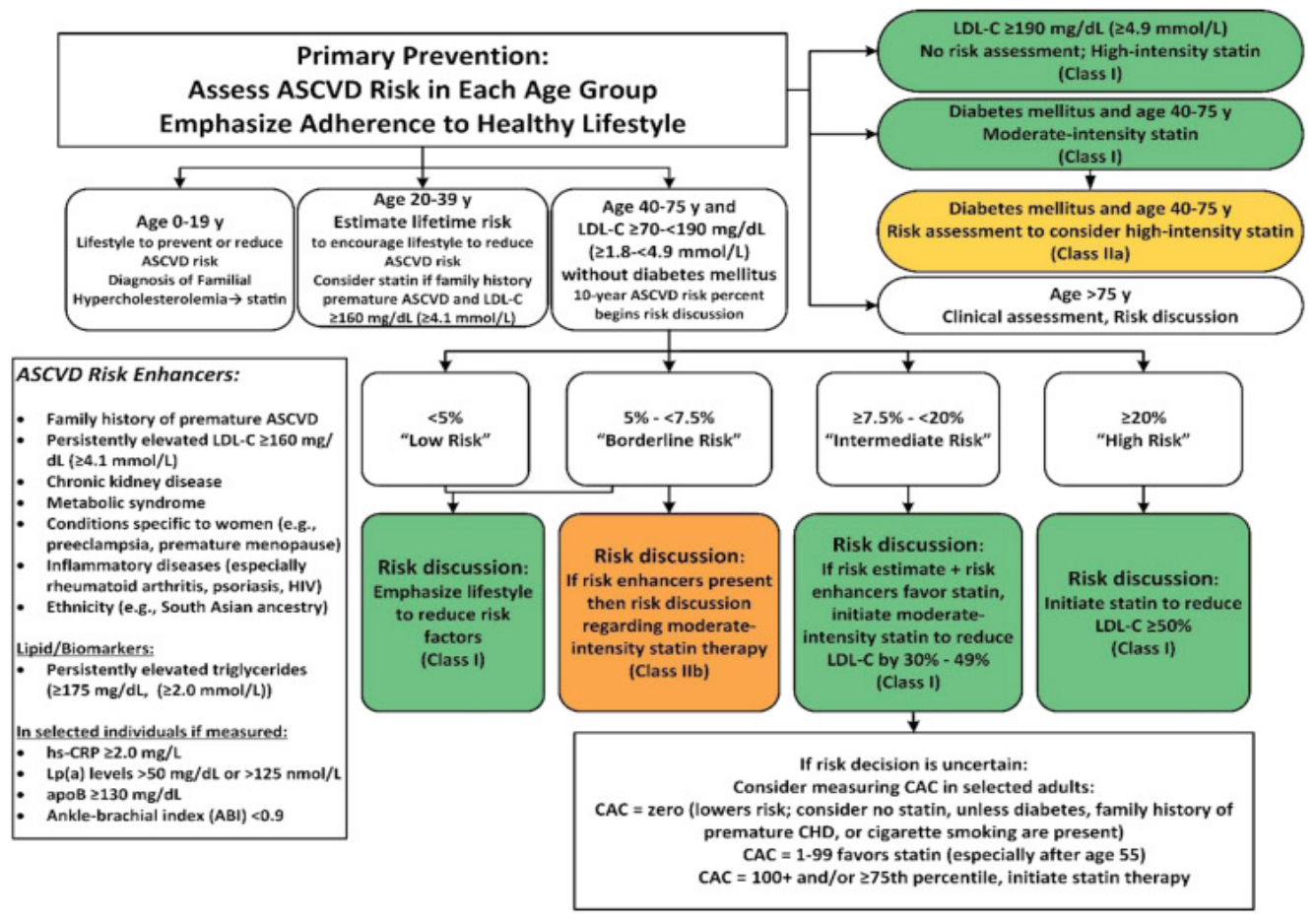
Figure from 2019 ACC/AHA Guideline on Primary Prevention of Cardiovascular Disease
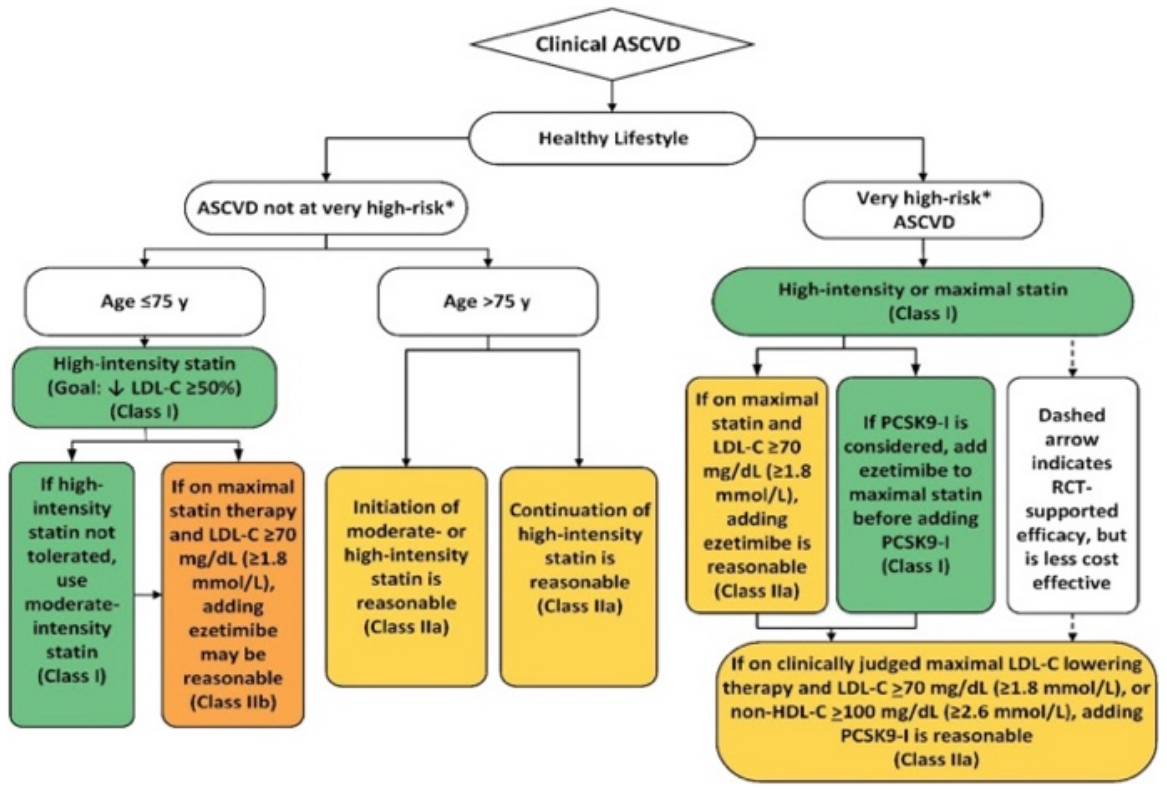
Figure from 2018 ACC/AHA Guideline on Management of Blood Cholesterol
| High Intensity (Decr LDL-C by > 50%) |
Moderate Intensity (Decr LDL-C by 30% - 49%) |
Low Intensity (Decr LDL-C by <30%) |
|---|---|---|
Atorvastatin (40mg) 80mg Rosuvastatin 20mg (40mg) |
Atorvastatin 10mg (20mg) Rosuvastatin (5mg) 10mg Simvastatin 20 - 40mg |
Simvastatin 10mg |
Pravastatin 40mg (80mg) Lovastatin 40mg (80mg) Fluvastatin XL 80mg Fluvastatin 40mg BID Pitavastatin 1-4mg |
Pravastatin 10-20mg Lovastatin 20 mg Fluvastatin 20-40mg |
|
| *Bold denotes dosing with RCT proven LDL lowering benefit | ||
Statin Options¶
Statin Side effects:¶
-
Spectrum of statin associated muscle symptoms (SAMS) include myalgias, myopathy, rhabdomyolysis, autoimmune myopathy
- Myalgias: bilateral involving large muscle groups, onset within weeks of initiation of therapy and should resolve within weeks of cessation; CK should be normal
-
Consider evaluation with CK, BMP, TSH, and vitamin D
-
ACC has a “Statin Intolerance Calculator” to help assess etiology of symptoms
Additional Information¶
-
If patient is not tolerating a statin, consider:
-
Holding statin until symptoms resolve and trialing lower dose or alternative statin (Pravastatin and Fluvastatin may have lower risks of myopathy)
-
Every other day dosing with atorvastatin and rosuvastatin (longer half-lives)
-
-
If repeated failed attempts, consider alternative agents: Ezetimibe, PCSK9 inhibitor
-
PCSK9 inhibitor requires referral to Lipid Clinic
Hypertriglyceridemia:¶
-
Moderate: TG 175-499 mg/dL; Moderate-severe 500 - 999; Severe: TG > 1000
-
Focus on addressing lifestyle factors and stopping medication that increase TG’s (HCTZ, some BB’s, estrogens, some ART, antipsychotics)
-
Consider medical therapy when TG> 500mg/dL (increased risk of pancreatitis):
-
Omega-3-fatty acids (icosapent ethyl) 4gm daily or Vascepa 4gm daily
-
Fibrates: Fenofibrate 120 mg daily (avoid in CKD), Gemfibrozil 600mg bid (increased risk of myopathy with concomitant statin)
-
VA-Specific Guidelines¶
-
https://www.healthquality.va.gov/guidelines/cd/lipids/index.asp
-
Lowest LDL goal recognized for VA Criteria for Use is 100
-
Preferred statins: Atorvastatin, Simvastatin, Lovastatin
-
Statins that require PADR: Pravastatin, Rosuvastatin (2nd line high intensity statin)
- Must have documented intolerances or drug-drug interaction to all preferred statins
-
Other agents that require PADR:
-
Ezetimibe
-
Pt has tried and failed or not tolerated all statins (allergy, AE, etc.)
-
Pt not meeting goal on max dose of statin PLUS bile acid sequestrants or niacin
-
-
Fenofibrate
-
Pt has tried all formulary alternatives or has contraindication to use of formulary alternatives (statin, niacin, gemfibrozil, cholestyramine, fish oil)
-
If TG > 500 mg/dL, fenofibrate should be approved
-
-