Consults for Radiology Procedures¶
- Radiology Procedures are performed by 3 separate consult services depending on the procedure requested.
- These pagers are covered 24/7, often by the same person for up to a week at a time (home call, not night float), so kindly reserve overnight pages for true urgent/emergent indications and save non-emergent communications until the morning
| Consult Service | Vascular IR | CT/US Procedures | Fluoro/Neuro/MSK fluoroscopy |
|---|---|---|---|
| EPIC Order | “Inpatient Consult to Interventional Radiology” | “Inpatient Consult for Adult Image-Guided Procedures (CT/US)” | Call 20878 (Fluoroscopy) for scheduling & orders. |
| Contact Number (weekdays) | #20840 (MD desk) |
#20120 (MD desk) |
#20878 (Fluoro techs) |
| Contact Number (nights & weekends) | Pager only | Pager only | #37185 (ER reading room) |
| Service Pager | 835-5105 | 835-0770 | N/A |
| Procedure Requested | -Active bleeding Embolizations -Cholecystostomy -PTC (biliary drains) -Nephrostomy -Tunneled lines -Dialysis interventions -G-tube placement -IVC Filter -Drain repositioning |
-Abscess drainage -Biopsies -Paracentesis** -Thoracentesis** |
-Dobhoff tube placements** -Lumbar punctures** -Joint injections / aspirations -Esophograms -Upper GI Series -Small bowel follow-through -Contrast enemas |
**Requires failed bedside/Inpatient medicine procedures service attempt
Specific Procedural Questions
Pre-Procedure (contact consult services for case-specific requirements, guidelines below):
-
NPO @ MN prior to procedure if sedation is to be used (majority of cases). Local only cases do not require patient to be NPO (see IR or CT/US procedures consult note for details).
-
Labs required within 1 month of procedure or sooner if there is a clinical situation that can affect those lab values. Think Warfarin and INR, for example.
-
INR (\<1.5 for most procedures)
-
Platelets (>50K)
- Anticoagulation
-
Google “SIR anticoagulation guidelines 2019”
-
VUMC IR guidelines based on SIR 2019 guidelines are included at end of section
Inpatient biopsies for malignancy: Inpatient biopsies are lowest priority on the CT/US procedures service given resource availability and will more than likely get bumped. We recommend that these get scheduled outpatient.
- Place an outpatient consult to image guided procedures at time of discharge/through discharge tab in EPIC to facilitate outpatient biopsies.
Drain Management
- Best to discuss directly with service that placed the drain (IR vs. CT/US vs. surgery)
- Flush with 10 mL sterile saline q shift while inpatient (flush into drain towards the patient and then place back to gravity or accordion suction bag)
- If drain output decreases, either:
-
The collection (e.g., abscess) has been drained
-
The drain is clogged/malfunctioning/mispositioned
-
Start with making sure there are no kinks in the drain, the 3 way is not clogged, and that the accordion drain is functioning.
-
Next, ensure the drain flushes appropriately. What this means is: you can flush the drain with 10 ml of saline and when you place back to gravity/accordion drainage bag you get back what you flushed in. There should be no leakage around the drain at the skin at baseline or during flushing.
-
If the drain is functioning, and there is still no output, obtain a CT w/ IV contrast to evaluate the collection and ongoing need for drainage,
-
If the collection remains, and drain is appropriately positioned within the drain, it is likely clogged/malfunctioning. First ensure proper suction/3-way direction. If this is not the issue, you can consider instilling tPA into the catheter for 2 hours
-
Would avoid in the setting of therapeutic anticoagulation given increased risk of bleeding unless discussed with procedural service).
-
Epic order: Alteplase (TPA) injection/infusion options Percutaneous drainage 2mg or 4mg
-
-
If this doesn't improve output in 48 hours, consider repositioning drain (VIR consult)
-
Anticoagulation for IR Procedures¶
Based on 2019 SIR Consensus Guidelines. JVIR 2019; 1168-1184. The length of time anticoagulation is held may differ from these guidelines in certain clinical circumstances at the discretion of the proceduralist. Generally, may resume anticoagulation 24 hours after the procedure.
Low Risk Procedures
- Screening coagulation laboratory tests
- PT/INR, platelet count, Hgb not routinely needed
- Suggested laboratory thresholds for most patients
-
INR: correct to \<3.0
-
Platelets: transfuse if \<20,000
- Suggested laboratory thresholds in patients with chronic liver disease
-
INR: n/a
-
Platelets: transfuse if \<20,000
-
Fibrinogen: cryoprecipitate if \<100
| List of Low-Risk Procedures | Medication | Action |
|---|---|---|
Vascular - Central venous catheter non-tunneled/tunneled line placement, removal and exchanges (e.g. port) - Dialysis assess interventions (e.g. shuntograms) - Gonadal vein embolization - IVC filter placement and retrieval - Laser ablation and phlebectomy - Lymphangiogram - Sclerotherapy for venous malformation - Transjugular liver biopsy - Venography and select venous interventions (e.g. adrenal vein sampling) Nonvascular - Superficial abscess drainage - Catheter exchanges (e.g. biliary, nephrostomy, abscess) - FNA/superficial biopsy - Gastrostomy and GJ exchanges - Appendicular skeleton bone biopsy, joint injections, peripheral nerve blocks - Thoracentesis - Paracentesis - Tunneled drainage catheter placement |
Anticoagulants | |
| Warfarin (Coumadin) | Target INR <3.0. Withhold 5 days for MSK procedures only. Bridging per PCP/cardiology | |
| Heparin (unfractionated) | Do not withhold | |
| LMWH (therapeutic) | Do not withhold | |
| LMWH (prophylactic) | Do not withhold | |
| Rivaroxaban (Xarelto) | Do not withhold | |
| Edoxaban (Savaysa) | Do not withhold | |
| Fundaparinux (Arixtra) | Do not withhold | |
| Apixaban (Eliquis) | Do not withhold | |
| Argatroban | Do not withhold | |
| Bivalirudin (Angiomax) | Do not withhold | |
| Dabigatran (Pradaxa) | Do not withhold | |
| Antiplatelets | ||
| Aspirin (81 or 325 mg) | Do not withhold | |
| Clopidogrel (Plavix) | Do not withhold | |
| Prasugrel (Effient) | Do not withhold | |
| Ticagrelor (Brilinta) | Do not withhold | |
| Cangrelor (Kengreal) | Do not withhold | |
| NSAIDs | ||
Short-acting - Ibuprofen - Diclofenac - Ketoprofen - Indomethacin |
Do not withhold | |
Intermediate-acting - Ibuprofen - Diclofenac - Ketoprofen - Indomethacin |
Do not withhold | |
Long-acting -Meloxicam |
Do not withhold | |
| Glycoprotein IIb/IIIa Inhibitors | ||
Long-acting - Abciximab (ReoPro) |
Withhold 24 hours | |
Short-acting - Eptifibatide (Integrilin) - Tirofiban (Aggrastat) |
Withhold 4 hours | |
High Risk Procedures
- Screening coagulation laboratory tests
- PT/INR, platelet count, Hgb
- Suggested laboratory thresholds for most patients
-
INR: correct to \<1.8 (\<1.5 if neuro procedure)
-
Platelets: transfuse if \<50,000
- Suggested laboratory thresholds in patients with chronic liver disease
-
INR: \<2.5. (\<1.5 if neuro procedure)
-
Platelets: transfuse if \<30,000
-
Fibrinogen: cryoprecipitate if \<100
| List of High-Risk Procedures | Medication | Action |
|---|---|---|
Vascular - Angiography and arterial interventions (e.g. chemoembolization, renal embolization, uterine embolization) - BRTO/BATO - Catheter directed thrombolysis (e.g. DVT, PE, portal vein) - Complex IVC filter removal - Lymphangiogram with thoracic duct embolization - Portal vein interventions - Pulmonary artery malformation embolization - Transjugular intrahepatic portosystemic shunt (TIPS) Nonvascular - Ablations (e.g. cryoablation, microwave ablation, radiofrequency ablation) - Deep abscess drainage - Biliary interventions (new placement e.g. cholecystostomy) - Deep non-organ biopsy (e.g. retroperitoneal, pelvic, intra-abdominal) - New Gastrostomy and GJ tube placement - Axial skeleton biopsy, bone marrow biopsy - Neuro: epidural injection, facet block, LP, myelogram, vertebral biopsy - Solid organ biopsy (e.g. liver, kidney, lung) - Spine procedures - Urinary tract interventions (nephrostomy tube placement, ureteral dilation) |
Anticoagulants | |
| Warfarin (Coumadin) | Withhold 5 days, goal INR <1.8. Bridging per PCP/cardiology | |
| Heparin (unfractionated) | Withhold IV for 4 hours Withhold SQ for 6 hours |
|
| LMWH (therapeutic) | Withhold for 24 hours | |
| LMWH (prophylactic) | Withhold for 12 hours | |
| Rivaroxaban (Xarelto) | Withhold: 2 days (CrCl>30) 3 days (CrCl<30) |
|
| Edoxaban (Savaysa) | Withhold 2 days | |
| Fundaparinux (Arixtra) | Withhold: 2 days (CrCl>50) 3 days (CrCl<50) |
|
| Apixaban (Eliquis) | Withhold: 2 days (CrCl>50) 3 days (CrCl<50) |
|
| Argatroban | Withhold for 2 hours | |
| Bivalirudin (Angiomax) | Withhold for 2 hours | |
| Dabigatran (Pradaxa) | Withhold: 2 days (CrCl>50) 3 days (CrCl<50) |
|
| Antiplatelets | ||
| Aspirin (81 or 325 mg) | 81mg: Do not withhold 325mg: Withhold 5 days unless angiography or neuro procedure |
|
| Clopidogrel (Plavix) | Withhold 5 days unless angiography/embolization | |
| Prasugrel (Effient) | Withhold 7 days | |
| Ticagrelor (Brilinta) | Withhold 5 days | |
| Cangrelor (Kengreal) | Avoid; if emergent withhold 1 hour | |
| NSAIDs | ||
Short-acting - Ibuprofen - Diclofenac - Ketoprofen - Indomethacin |
No recommendation | |
Intermediate-acting - Ibuprofen - Diclofenac - Ketoprofen - Indomethacin |
No recommendation | |
Long-acting -Meloxicam |
No recommendation | |
| Glycoprotein IIb/IIIa Inhibitors | ||
Long-acting - Abciximab (ReoPro) |
Withhold 24 hours | |
Short-acting - Eptifibatide (Integrilin) - Tirofiban (Aggrastat) |
Withhold 4 hours | |
Contrast Allergies or Extravasation¶
See ACR contrast manual for additional Information:
https://www.acr.org/Clinical-Resources/Contrast-Manual
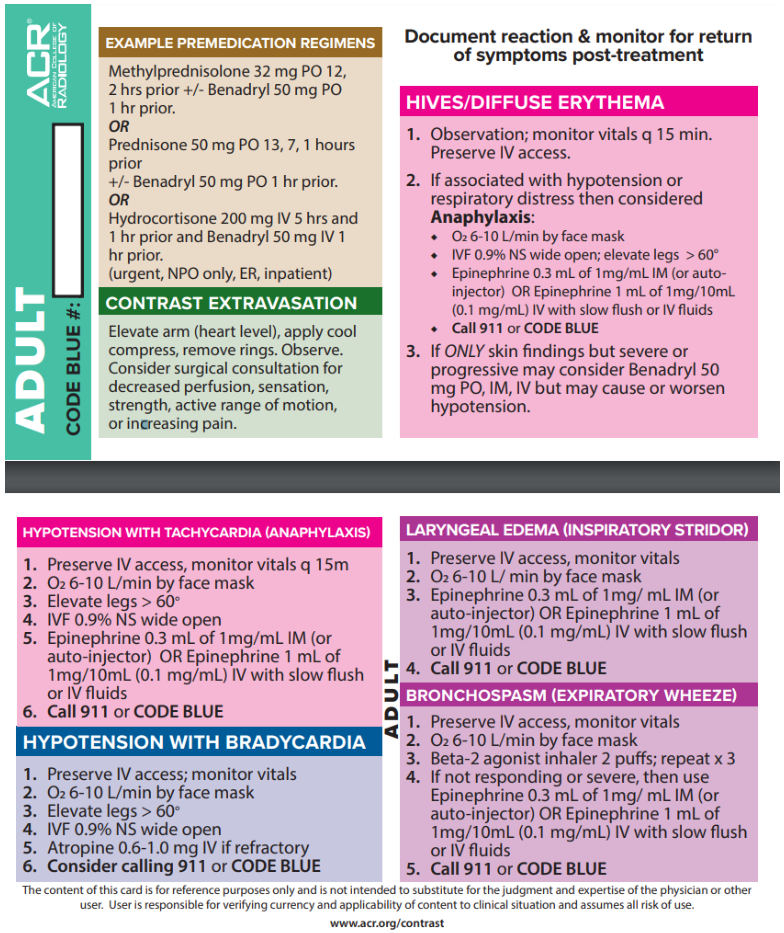
From the ACR contrast manual